Abstract
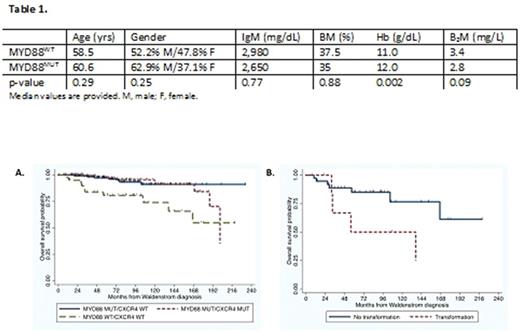
Activating mutations in MYD88 and CXCR4 are present in 93-95% and 30-40% of patients with Waldenstrom's Macroglobulinemia (WM), respectively. Mutations in MYD88 trigger NF-KB dependent growth and survival of WM cells through BTK/IRAK, and AKT/ERK through HCK (Yang et al, Blood 2013; 2016). Patients with MYD88 mutations show high levels of response activity to ibrutinib, that targets BTK and HCK, while responses are poor in MYD88WT patients denoting biological differences between these two subgroups (Treon et al, NEJM 2015). The mutational landscape of MYD88 wild-type (WT) patients is under investigation, though is likely to involve alternative signaling pathways based on transcriptome studies (Hunter et al, Blood 2016). In a previous study, we observed that patients with MYD88WT were at higher risk of death, while CXCR4 mutation status had no impact on overall survival (Treon et al, Blood 2014). Given the uncommon nature of MYD88WT WM disease, we sought in this study to investigate the impact of MYD88WT status in a larger population of WM patients. WHO and WM Consensus guidelines were utilized to establish WM diagnosis, and thorough pathological and laboratory testing was undertaken to exclude non-WM IgM secreting B-cell entities. We utilized sorted CD19+ lymphoplasmacytic cells (LPC) obtained from the bone marrow of WM patients, and determined MYD88 mutation status by highly sensitive and specific AS-PCR for MYD88L265P as before (Xu et al, Blood 2013). Patients with wild-type MYD88 by AS-PCR underwent Sanger sequencing to exclude non-L265P MYD88 mutations as before (Treon et al, NEJM 2015). CXCR4 mutation status was determined in sorted LPC by AS-PCR and Sanger sequencing as before (Xu et al, BJH 2016). We identified 46 MYD88WT WM patients by these efforts, and compared their findings at time of diagnosis, and survival outcome to 262 patients with MYD88 mutated (MYD88MUT) disease who were diagnosed over the same time-period. The median follow-up for all patients was 74.7 (0.5-324.9 months), and was similar for MYD88WT and MYD88MUT WM patients (64.1 vs. 73.7 months, respectively; p=0.71). Patient characteristics are shown in Table 1.
Among 262 MYD88MUT patients, 261 had L265P and 1 had the S243N MYD88 mutations; 101 (38.5%) were also CXCR4 mutated. Four (8.6%) MYD88WT patients were also CXCR4 mutated. During the follow-up period, there were 11 (23.9%) and 15 (5.7%) deaths among the MYD88WT and MYD88MUT patients (p=0.003). Figure 1A shows overall survival based on MYD88 and CXCR4 mutation status from time of diagnosis for all patients. The estimated 10-year survival was 73% (95% CI 52-86%) and 90% (95% CI 82-95%) for MYD88WT and MYD88MUT patients, respectively (Log-rank p<0.001), and did not differ for MYD88MUT patients by CXCR4 mutation status (Log-rank p=0.69). Multivariate analysis that included age, gender, serum IgM, hemoglobin, BM disease involvement, serum B2M, MYD88 and CXCR4 mutation status only showed MYD88 mutation status (p<0.001) as a significant determinant for overall survival. Transformation to diffuse large B-cell lymphoma occurred in 7 (15.2%) and 2 (0.76%) of MYD88WT and MYD88MUT patients, respectively (p<0.0001), with odds ratio of transformation for MYD88WT versus MYD88MUT of 23.3 (95% CI 4.2-233.8; p<0.001). Among MYD88WT patients who transformed, overall survival was shorter (Figure 1B; Log-rank p=0.08).
Our findings affirm the prognostic significance for MYD88 mutation status as an important determinant of overall survival in WM, and identify a high risk of disease transformation in patients with MYD88WT disease.
Treon: Pharmacyclics: Consultancy, Research Funding. Castillo: Pharmacyclics: Consultancy, Research Funding; Abbvie: Research Funding; Millennium: Research Funding; Janssen: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal